Have we truly considered the barriers to point-of-care testing?
03 Apr 2018
Written by Rose Brade
In an announcement by Public Health England last year, it was claimed that ‘at least’ 20% of all antibiotic prescriptions are inappropriate. ‘Pester patients’ who place pressure on their GP to prescribe courses of antibiotics are frequently blamed. Such patients idealise antibiotics as ‘magic pills’, often believing that failure to obtain a prescription means that they are not ‘actually ill’. Whilst we are on a mission to halve the number of antibiotic prescriptions by 2020, there are still many barriers, to consider when introducing a tool to specifically drive down their use.
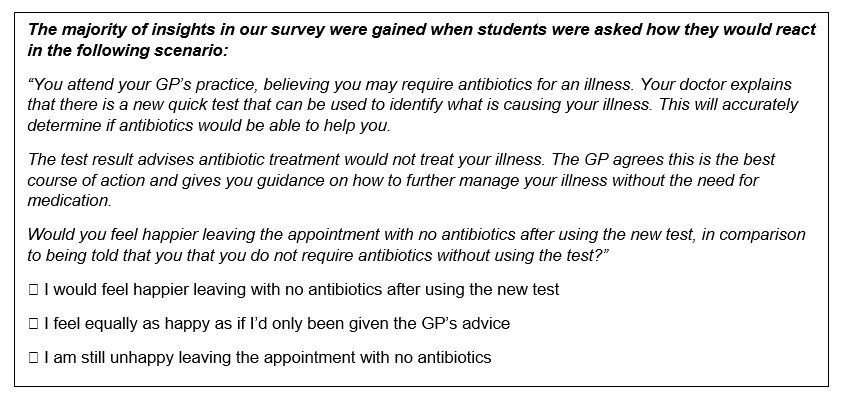
Using a survey, my team investigated how successful introducing a point-of-care test might be in a clinical setting. Would this be an effective way to reduce prescribing of antibiotics or would patients continue to hold onto their beliefs that without a prescription they were not “actually ill”?
Promising results?
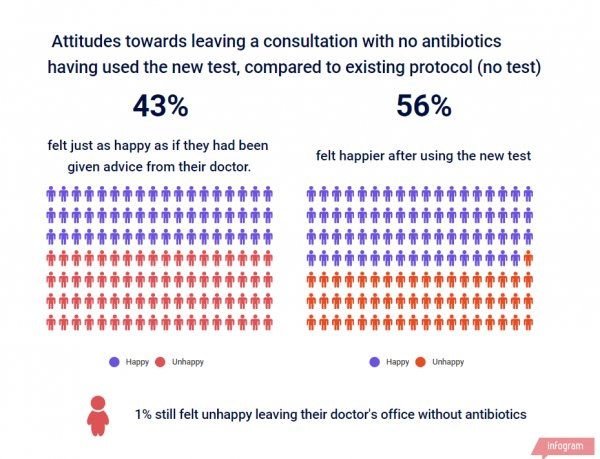
In our survey of 206 university students, we found that the diagnostic test successfully improved patient satisfaction in the absence of an antibiotic prescription:
56% of students agreed they would be happier leaving a consultation with no antibiotics (a 13% superiority achieved compared to feelings towards the existing diagnostic protocol).
Only 1% said that would still be unhappy.
Interestingly, 43% of respondents said they were ‘equally as happy’.
These results demonstrate initial promise, but worryingly amongst the 43%, who did not display a change in behaviour when the diagnostic test was used, results may suggest a lack of awareness around why the misuse of antibiotics is so important.
Limited knowledge of antimicrobial resistance = lower receptivity to point-of-care diagnostics
We separated the respondents by their pre-existing knowledge of antimicrobial resistance and antibiotic use, gauged from earlier survey questions, as we thought that perhaps increased awareness of antibiotic resistance may lead to higher levels of engagement in new diagnostic testing.
This was confirmed! Students with ‘more knowledge’ were on average more receptive to the test, likely due to understanding the advantage of having a biological test confirm diagnosis. .
Of the 16 respondents who reported they were ‘unhappy’ or ‘unsure’ of leaving without antibiotics in-spite of the test, 14 were considered as having ‘lower knowledge’ surrounding antibiotics and resistance. We found from these results that those with limited knowledge more closely resembled ‘pester patients’.
Taken together, our research therefore forecasts that point-of-care diagnostics in concert with public campaigns communicating their benefits, can make the greatest change in behaviour, and therefore will have the greatest benefit.
Those with limited knowledge of antibiotic resistance relayed that without adequately understanding what the new test achieves, it may lead them to question their GP’s ability. Raw commentary included, “Why should GPs require a machine? Do they not know what is wrong with me, did they not go to med school?” or “This seems like more faff and a waste of my time”. Indeed, one individual countered that the present protocol for diagnosis is adequate as “it’s not like cancer or something; I’m not going to die if they get it wrong.”
Greater knowledge may also hamper receptivity
Whilst the above rings true, the premise of this hypothesis did not consider that students with ‘more knowledge’ may question the validity of the test or its implications. This gives rise to an alternative hypothesis which may underscore a significant portion of the broader UK population. Whilst this was not a strong trend in our research, the limited cross-section of the sample may have influenced this.
It became apparent that the question of a patient accepting a test could not be evaluated based only on their knowledge of antibiotic resistance, but also needed to take into account the potential disease they are being tested for.
Concerns due to clinical validity do hold some weight. To date worldwide, diagnostics have had less impact on prescribing than anticipated, and this may be explained by failures in speed, accuracy and sensitivity. Further, false positive/negatives are a worry as simply detecting an organism is not necessarily clinically meaningful; many people harbour virulent microbes while remaining healthy.
Willingness to consent may depend on the severity of suspected illness
As our analysis became more in-depth, it became apparent that the question of a patient accepting a test could not be evaluated based only on their knowledge of antibiotic resistance, but also needed to take into account the potential disease they are being tested for. In the case of sepsis, the window for treatment is a few hours, and inappropriate treatment is far more dangerous compared to a non-complex respiratory tract infection. In these instances, both healthcare professionals and patients will usually prefer to ere on the side of caution, highlighting a significant degree of trust in the diagnostic is necessary for consistent use.
Other considerations that may affect opinions on diagnostic tests for antibiotic resistance
Fear of a lack of medicalisation– Several respondents commented that the diagnostic would “deter them from getting better as soon as possible”.
New test replaces doctor– This links to several lines of research which claim point-of-care tests may lead to clinicians treating the test rather than the patient, bypassing current assessment of clinical symptomology and inducing an over- reliance on test results.
Overall, there is a clear appetite and willingness to use point-of-care diagnostics
Limited effect– Another perceptive comment included that if point-of-care diagnostics were only launched in the UK, they would have a “limited effect” as “resistant bacteria can spread”.
What we suggest
Overall, there is a clear appetite and willingness to use point-of-care diagnostics. However, our research shows that there are barriers in the UK which may make it harder to roll-out a test. Therefore, it is important to consider various strategies and points of view when introducing a test; these must be explored from both clinical and behavioural perspectives in order to drive change and potentially reduce “pester patients”.
Trust within the doctor–patient relationship may lend to patients consenting simply if their clinician suggests. Healthcare professionals must therefore play an active role in communications around their roll-out.
Targeted public campaigns– those with ‘more knowledge’ were significantly more aware of antimicrobial resistance campaigns than those with ‘less knowledge.’ This strongly implicates public campaigns as the strategy to transition those from lower knowledge à greater knowledge and increase receptivity.
Prioritise antibiotic resistance in concert with other public health matters– Research revealed students felt it was less ‘visible’ compared to messaging around flu jabs, cancer and sexual health. Where possible, link the two e.g. gonorrhoea/HIV with superbugs.
Rose Brade is a health communications professional. Research was carried out at The University of Leeds as part of her final research project into student attitudes to rapid point-of-care diagnostics and the avoidance of antibiotic resistance. For further information, connect with Rose on LinkedIn: Rose Brade
