HIV and diagnostic tests: Aiming for undetectable status
01 Dec 2016
Written by Dr Teri Roberts
Teri is diagnostics advisor at the MSF Access Campaign, and member of our Prize Advisory Panel. Today is World AIDS Day, and we asked Teri to tell us about the role of diagnostics in HIV/AIDS treatment.
What HIV tests have been the real game-changers?
Rapid diagnostic tests, which measure antibodies to the HI-virus and can be performed at point-of-care, have been real game-changers for allowing people to find voluntary testing and counselling services closer to where they live and work.
Any test that facilitates community-centric and convenient solutions, without compromising quality, should be widely used to improve testing rates. On the back of this, self-testing should be used more frequently in the future.
Rapid diagnostic tests (RDT) based on voluntary counselling and testing (VCT) are widely used and the standard for HIV testing in most developing countries. Self-testing is newer and hasn’t yet been widely rolled out.
The more recent roll-out of viral load testing as the preferred monitoring test has also been game changing. Failure of antiretroviral therapy (ART) leads to a fall in CD4 count, but it takes a long time for this decrease to happen. By contrast, viral load is a measure of the level of HIV in the blood and thus functions as an immediate and cross-sectional measure of treatment effectiveness.
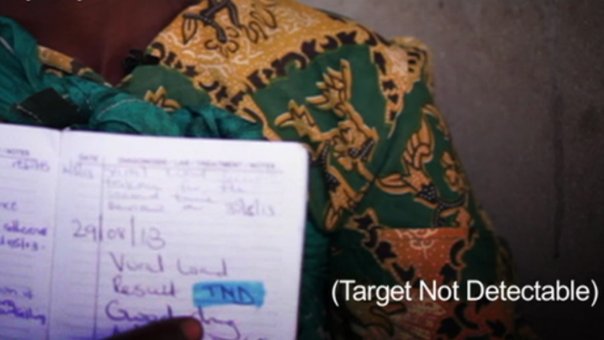
It is also quite a simple metric to interpret: if you’re undetectable your treatment is working. If your viral load is above 1000 copies/mL further intervention is needed for adherence, counselling and/or treatment switch, in the case of antimicrobial resistance. This allows for simplification of ART delivery as those remaining undetectable may access their ART through other care in the community, like community adherence groups, while only needing a clinical visit once a year (where they’ll have their viral load retested).
This in turn allows clinics to concentrate on those people needing clinical care while allowing healthy, stable people to avoid long queues and unnecessary clinical visits, particularly when people live far from the clinic or it is difficult for them to take leave from work.
Viral load scale-up is still in progress. Most countries have updated their guidelines to reflect the WHO recommendations of routine viral load testing for all those on ART, however implementation has been slow on the ground.
Why must HIV tests be rapid and efficient at the point of care (POC) to really make a difference?
POC testing makes the most difference when it is a diagnostic (as opposed to a monitoring) test. This is because at each stage of diagnosis and linkage to care there may be losses when people have to return for multiple visits to have a sample taken, return for their results, be prepared for treatment and finally start treatment.
This is even worse in the case of eligibility criteria (CD4 count for HIV) when people are told they need to come back at some point in the future to be reassessed for treatment eligibility. They may never return. ‘Test and treat’ is also the best approach for preserving people’s health. Using POC tests can avoid at least one gap in the so-called leaky cascade by providing an immediate test result and immediate linkage to care.
It is also important to use sample types like capillary whole blood, urine or swabs to easily access a sample. For example, in many healthcare clinics phlebotomy services are not available. Tests must also be stable at high temperatures and humidity, simple to perform and having a long shelf-life.
Lab-based testing can be difficult when the lab is far from the clinic or when the sample types needed (e.g. Vacutainer whole blood or plasma) are not feasible, either because they cannot be processed on site or because there is no transport efficient enough to get the sample to the lab in time for processing.
One way in which this has been overcome is to use dried blood spots (DBS), which can be used for serological and virological testing and are stable for a few weeks at ambient temperature once dried. They are also affordable, easy to transport, and may be prepared from capillary whole blood.
What similarities exist between HIV diagnostic tests and the test we’re looking for with the Longitude Prize?
All the criteria for the Longitude Prize reflect the type of tests we need in resource limited settings. In fact, more and more we are seeing that innovative tests and solutions to meet the needs of developing countries will also be useful in high income countries, including issues of affordability while retaining quality and accuracy.
On the connectivity need, although not widely implemented, it is clear that this is an important advantage for POC tests so that they can be linked to lab information management systems (LIMS) for monitoring. This includes quality assessment, patient results (especially useful when people move between clinics, often the case with chronic diseases), epidemiological surveillance and stock management.
What key message do you want to relay to people on World AIDS Day today?
Undetectable! If your viral load is undetectable, your treatment is working.
The ultimate goal of ART is that all people are able to safely, conveniently and frequently test for HIV; that those who are HIV infected are able to access lifelong therapy; and that treatment be switched when there is resistance. Since the development of combination ART, HIV/AIDS is no longer a death sentence. 18 million people living with HIV in the resource-limited world are receiving treatment. However, with 1.1 million HIV-related deaths, and 2.1 million new infections in 2015, the end of AIDS is not in sight.
Image credit: Greg Lomas/MSF
