In the balance: GPs, patient care and antibiotics
19 Aug 2014
Written by Dr Rosemary Leonard
Antibiotics are the backbone of modern medicine and have been our best form of defence against bacterial infection for over 80 years. However, it is clear that certain infectious bacteria we once treated so effectively with antibiotics are now becoming resistant to those drugs, with the World Health Organisation saying that antibiotic resistance ‘is now a major threat to public health’.
With over 41 million antibiotic items dispensed in the community in England alone in 2013, what part do the General Practitioners – the doctors prescribing drugs in our communities up and down the country – currently play in their ongoing effectiveness?
In the recent survey on behalf of the Longitude Prize, 49% of GPs say they prescribe antibiotics once a week or more without knowing whether they are medically necessary, and 72% GPs prescribe antibiotics when they are unsure if they are treating a viral or bacterial infection.
Why might this be?
GPs are on the front line of healthcare in the UK, and the responsibility that lies with them is huge. The trust put in GPs (78% of patients surveyed say they trust their GP to diagnose their condition accurately) represents our greatest responsibility – duty of care for our patients. A doctor’s main concern is to improve the health of their patient and often prescribing antibiotics as a cautionary measure is the safest way to achieve this without an easy way to tell if an infection is bacterial or viral.
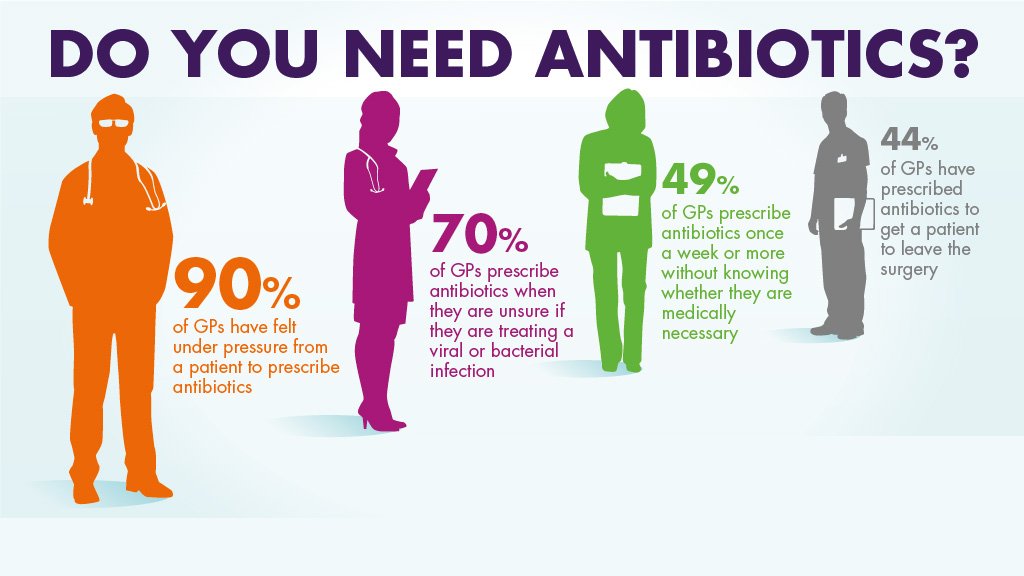
In the responses to the Longitude Prize’s survey many GPs also aired the view that they lacked time to deal with persistent patients, and that they feared complaints if they did not immediately prescribe the treatment a patient might need. In general it is very positive to see that most patients understand how and why they should be prescribed antibiotics so while some education is still needed (36% of respondents in the survey thought that antibiotics could be used to treat a virus), much of the pressure is on GPs to prescribe antibiotics correctly and not simply give patients peace of mind by prescribing a drug without a thorough diagnosis.90% of GPs feel that they are pressured into giving antibiotics by their patients. Gaining the confidence to know the type of bacteria or pathogen with improved diagnostics could be invaluable. It could give them extra knowledge to know when to prescribe and when not to, or what type of antibiotic would be best to target a specific bacteria. Diagnostics can also provide a valuable role in collecting data about bacteria and contributing the global surveillance effort.
There are a wide range of factors that can help slow resistance to antibiotics, from the public’s attitude towards them and the healthcare system to the amount of funding put towards helping developing new antibiotics and effective diagnostics.
The incentive provided by the Longitude Prize will hopefully reap fantastic rewards for the medical world.
